10 simple tips for preventing AMD
As people age, several conditions can develop, affecting their general well-being. Of these, age-related macular degeneration is common in people over 50. The condition leads to vision problems due to severe degradation of the focal area of the retina, known as the macula. The macula is responsible for focused vision. Macular degeneration affects central vision and the ability to recognize faces, use a computer, or watch television. Here is how one can prevent the condition:
Wear sunglasses
Regularly putting on sunglasses while stepping out can help one protect their eyes. Excessive sun exposure for prolonged periods increases the risk of age-related macular degeneration (or AMD). Additionally, looking directly at bright sunlight, even for a short period, can cause permanent damage to the retina. Sunglasses that bear a UV400 protection label are excellent options. Further, one should always wear sunglasses when stepping out to prevent making their eyes vulnerable to vision-related issues. If one spends a lot of time in the sun, they should also wear a wide-brimmed hat to protect the eyes from UV rays. Additionally, as age-related macular degeneration can develop in people who have had excessive exposure to sunlight, one should avoid looking directly at the sun during peak daylight. Those who spend a lot of time using digital devices should consider taking a break every 20 minutes and looking away from the screens to reduce strain on the eyes. It is also important to limit the use of blue-light devices before going to bed to maintain eye health.
Add fish to meals
Age-related macular degeneration is less common in people who add fish to their meals. This is because fish like sardines, trout, as well as salmon are rich in omega-3 fatty acids, which are known to exhibit anti-inflammatory properties. So, foods rich in omega-3s can help reduce inflammation, increasing the risk of AMD. Additionally, both fish and fish oil are known to serve as strong prevention against the disease.
Make better food choices
One’s nutritional regimen can play an important role in preventing age-related macular degeneration. So, one should ensure that their daily meals contain good portions of vegetables, fruits, seeds, and fresh meats. Dark and leafy vegetables like spinach, kale, and broccoli, are known to lower the risk of AMD as the veggies are rich in carotenoids like lutein, a type of phytonutrient that has antioxidant properties, protecting the body from diseases. Additionally, it is also important to opt for foods rich in omega-3 fatty acids to slow down the progression of AMD. In addition to fish, walnuts, seeds, and nuts can also be great sources of omega-3s. It is also important to choose antioxidant-rich fruits like strawberries and blueberries, as they can protect the eyes against free radicals. Apart from adding nutrient-rich food, one should avoid excessive intake of refined carbohydrates as it is known to elevate the risk of eye-related issues.
Consider taking supplements
People who are not able to get the required nutrients through their meals can be affected by nutrient deficiencies that can affect their overall health. Taking multivitamins and other supplements on the recommendation of a doctor can boost one’s health, deal with deficiencies, and prevent diseases like age-related macular degeneration. Further, certain vitamins are also known to slow the progression of eye-related conditions.
Adopt an active lifestyle
People who have a high-fat meal plan and lead a sedentary lifestyle have an increased risk of getting age-related macular degeneration. Indulging in any kind of physical activity like walking, running, or swimming on a regular basis can help in maintaining a proper physique and staying healthy. Exercising can also help one maintain and improve their eyesight.
Keep blood pressure and cholesterol in check
People with hypertension may have a higher chance of developing age-related macular degeneration, as high blood pressure tends to restrict the normal flow of blood to the eyes. Hypertension or high blood pressure can be brought on by several factors like less physical activity, unhealthy lifestyle, and genetics. Introducing healthy changes to one’s daily meal plans, like including fruits and vegetables rich in vitamins, minerals, and antioxidants, and performing any kind of physical activity can aid in maintaining cardiovascular as well as eye health.
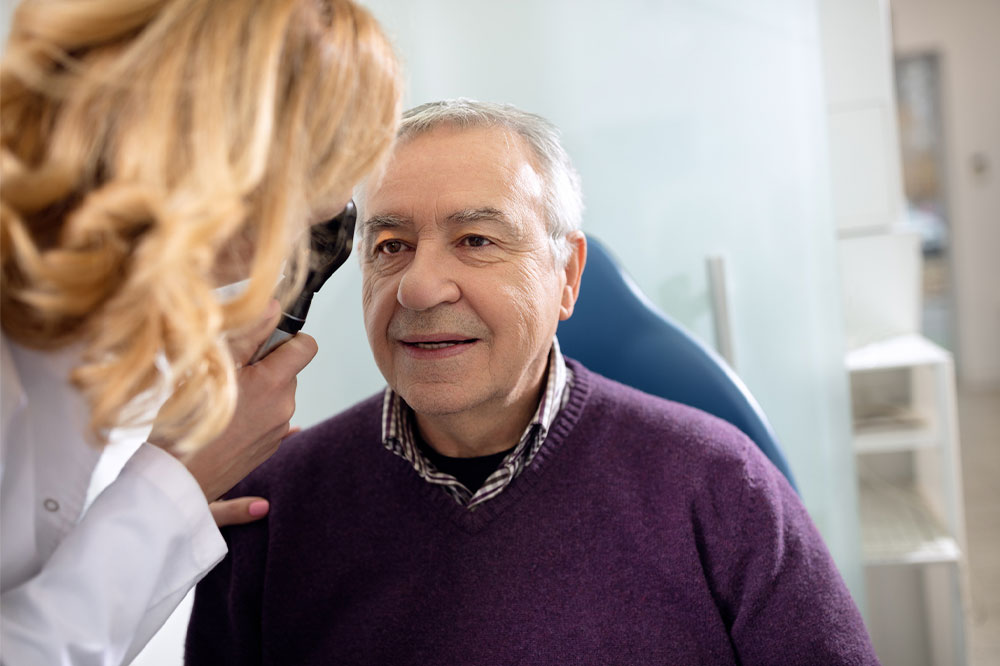
Get regular eye check-ups
Age-related macular degeneration, when detected early, can be slowed down by making lifestyle changes and using treatment options. So, getting one’s eyes checked regularly can help doctors detect potential issues or existing conditions and recommend corrective measures. Further, AMD may not cause visible symptoms in the early stages, however, a specialist can detect minor changes in the eye and vision during an eye examination and can offer a precise diagnosis. So, early detection of the condition can help in preventing vision loss by managing the condition and its progression.
Follow the doctor’s instructions
People who have been taking certain supplements or prescription treatments to manage their cholesterol and blood pressure levels should not miss their dose or stop the treatment. Controlling these risk factors can help reduce the risk of developing age-related macular degeneration.
Check for a family history of the disease
People with an immediate family member affected by age-related macular degeneration can be at a higher risk of developing the disease. So, one should recognize this risk factor and learn about early signs, prevention, and management of AMD. Understanding the condition can help one detect symptoms like problems in recognizing faces, difficulty adapting to low-light conditions, and issues with seeing straight lines.
Try self-assessment
Those who believe they have age-related macular degeneration can try checking their vision by opting for an at-home test. One can use a testing tool known as the Amsler grid, which is used by specialists to recognize potential issues connected to macular degeneration. The test requires one to look at a paper grid and if one observes their central vision in one or both eyes has become darker and the grid lines appear wavy, then they may have AMD. This conclusion, however, should be confirmed by a doctor after conducting an official eye examination.

